Step 1 : Select At Least 1 Outcome Measure
For the MIPS Quality Performance Category, you must report at least one outcome measure. If no outcome measures are applicable to your patient population, then you must select at least one high-priority measure (see Step 2). The outcome measures you report do count towards the six measure requirement for the Quality Performance Category.
Show Recommended Outcome Measures
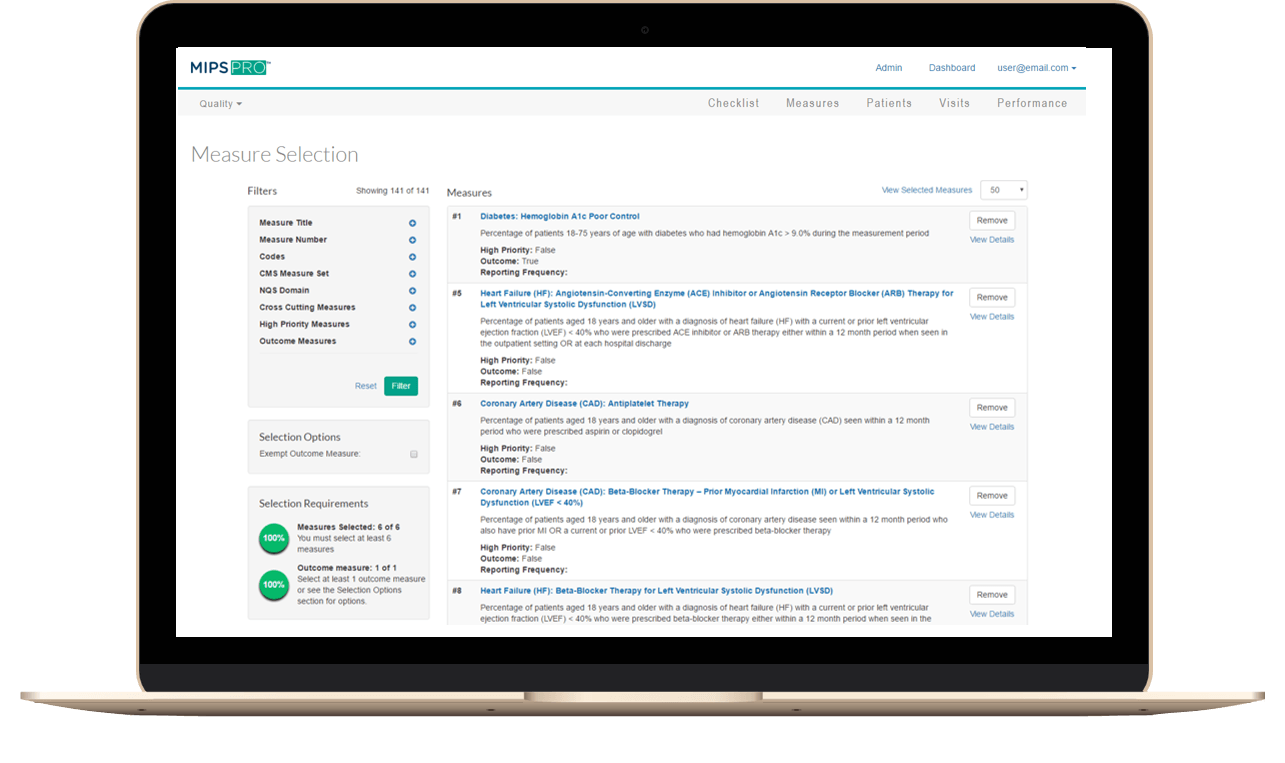
Step 2 : Select Applicable High-Priority Measures
If you were able to select an outcome measure in Step 1, this step is optional. High-priority measures are worth bonus points for the Quality Performance Category. This makes it a smart idea to include as many high-priority measures as possible in your six Quality Performance Category Measures.
Show Recommended High-Priority Measures
Step 3 : Make Sure You Have 6 Measures Selected
If you have not yet selected six measures and are aiming for a positive MIPS Payment Adjustment, select from the other recommended measures. Reporting at least one measure successfully will qualify for avoiding the MIPS penalty. If you report over six measures, CMS will calculate your MIPS Quality Performance Score using your top performing quality measures.